The human body is home to trillions of microorganisms that play a significant role in our health, and we already know that consuming some bacteria as a supplement – popularly known as probiotics – can have health benefits such as improved digestion.
But according to new research spearheaded by Irish psychiatry professor Ted Dinan, human bacteria may be even more influential than previously thought. What Dinan and his fellow researchers suggest is that certain bacteria may have a direct impact on brain function.
Ingesting these “psychobiotics” – as the researchers call them – could not only be a groundbreaking therapy for mental disorders such as depression, but may also have nootropic activity that could enhance cognitive function.
Microbiota in the Gut – a Beneficial Relationship
According to recent estimates, the human body contains 39 trillion bacteria and 30 trillion human cells.1 Although these figures are a far cry from the 10:1 microbe to human cell ratio that was previously suggested, one fact remains certain – bacteria play an important role in human health.
The large majority of these microbiota reside in the intestines in a complex community of more than 1000 different species and 7000 strains.2
Here, the bacteria serve a number of well-established functions such as producing nutrients that our bodies cannot make themselves, and influencing immune system responses. But as recent research suggests, they also have a major impact on the brain and behavior.
The Gut-Brain Axis
![Gut-Brain Axis illustration. By HDThink (Own work) [CC BY-SA 4.0], via Wikimedia Commons](https://supplementsinreview.com/wp-content/uploads/2016/07/DIAMOND_Proposed_Mechanism_of_Action.png)
One key breakthrough is the idea that intestinal bacteria can impact the so-called gut-brain axis – the biological communication that occurs between the brain and the gastrointestinal tract via nerves, hormones, and other pathways. In fact, microbiota are now seen so central to this axis that researchers recently coined the term “microbiome–gut–brain axis”.3
One of the most compelling pieces of evidence for the existence of this axis is irritable bowel syndrome (IBS) – a common gut disorder which can cause both digestive and mental symptoms.
Moreover, clinical trials demonstrate that boosting levels of probiotic bacteria in IBS patients can improve anxiety, providing solid proof that such psychobiotics are able to influence mental health via the axis.4
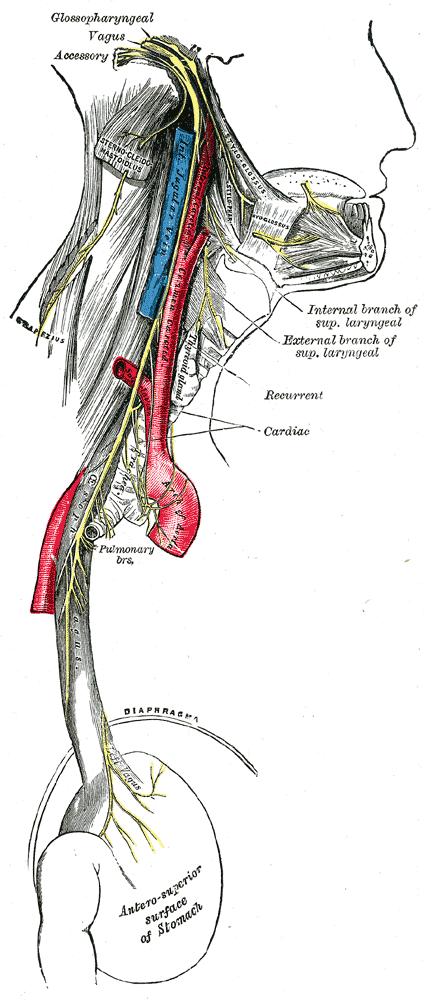
The Vagus Nerve
The discovery of the microbiome-gut-brain axis raises an important question – how exactly can bacteria influence the brain from the gastrointestinal tract? One possible answer is via the vagus nerve, which runs down from the brain to the gut.
This idea was demonstrated in a 2011 study, where Dr. Dinan and his colleagues gave mice either normal, or food fortified with probiotic Lactobacillus rhamnosus bacteria.
They found that mice given the probiotic had reduced anxiety, depression, and a healthier response to stress, which was associated with altered brain levels of the GABA receptor – a protein that detects and responds to the neurotransmitter GABA. They also found that mice with a severed vagus nerve did not have any of the above benefits.6
Mechanisms of Action
Researchers believe that psychobiotic bacteria work via three main mechanisms: producing neurotransmitters, regulating the body’s stress response, and influencing the body’s response to inflammation.
Producing Neurotransmitters
One of the leading hypotheses for how psychobiotics might influence the brain is by producing neurotransmitters – compounds that are used by nerve cells to send signals. Neurotransmitters are crucial to brain health and their dysfunction has been associated with a large variety of mental disorders, ranging from depression to Alzheimer’s.
Although current evidence is limited to animal and petri dish studies, the findings are promising:
- Certain strains of Lactobacillus and Bifidobacterium bacteria are able to produce the neurotransmitter gamma-aminobutyric acid (GABA).7
- Some subspecies of Lactobacillus can produce acetylcholine, yet another important neurotransmitter8
- Blood levels of serotonin – a neurotransmitter particularly involved in mood and behavior – are substantially higher in healthy mice, compared to those with no gut microbiota9
- The brains of germ-free (lacking gut microbiota) mice appear to have significantly lower levels of norepinephrine and serotonin10
- Some bacterial strains are also capable of producing the catecholamines norepinephrine and dopamine8
More on nootropics that help with neurotransmitters
Regulating the Stress Response

Research suggests that gut bacteria play an important role in regulating this axis, and its dysfunction appears to be linked to the development of stress-related disorders such as depression.12
For example, as one frequently-cited study demonstrated, inducing mild stress in mice with no gut microflora causes a stronger release of stress hormones than in their healthy counterparts. In addition, transplanting healthy bacteria into the mice appeared to reverse this elevated response to stress.13
Meanwhile, another study reported that separating infant rats from their mothers early in life not only altered their microbiota, but also resulted in increased anxiety and stress hormone levels. Researchers suggest that this kind of early-life stress could contribute to the development of psychiatric disorders – such as depression – upon reaching adulthood.14
Moreover, a study in human participants showed that supplementation with a probiotic containing Lactobacillus helveticus R0052 and Bifidobacterium longum R0175 was able to not only able to reduce levels of cortisol – the main stress hormone – but also eased psychological distress.15
More on anti-stress nootropics
Regulating the Inflammation Response
The third potential mechanism of psychobiotic bacteria is modulation the body’s response to inflammation. In particular, recent research suggests that production of inflammatory molecules known as cytokines may be associated with depression, anxiety, and stress.16
In turn, there is evidence that gut bacteria are capable of reducing this inflammation or altering how the body responds to it.
For instance, one study demonstrated that giving probiotic bacteria to germ-free mice promoted the production of regulatory T cells, which play a role in preventing and limiting autoimmune and inflammatory disorders. But more importantly, the probiotic also promoted synthesis of IL-10, an immunoregulatory cytokine that suppresses inflammation and is believed to be one of the ways that antidepressants work.171819
Similarly, a study in pregnant women showed that a Lactobacillus GG probiotic is also capable of stimulating IL-10 release.20
Psychobiotics Research Evidence
Although the vast majority of research is currently limited to rodents, psychobiotics is quickly growing to become one of the most popular areas of clinical research. With more and more human trials being undertaken every year, the possibility of being able to take psychobiotic pills to cure a bout of depression or even boost mental performance may soon become a reality.
Animal Research
- Lactobacillus plantarum PS128 consumption in mice appears to improve symptoms of anxiety and depression, reduce levels of inflammatory cytokines, and normalize the stress response2122
- Anxious mice given a probiotic containing Bifidobacterium longum 1714 and Bifidobacterium breve 1205 had reduced anxiety and improved cognitive performance2324
- Rats subjected to stress for 21 days and supplemented with either an SSRI antidepressant or Lactobacillus helveticus NS8 saw a reduction in anxiety, depression, and cognitive decline; the probiotic was found to be more effective than the antidepressant25
Human Research
- Eight weeks of probiotic treatment containing Lactobacillus acidophilus, Lactobacillus casei, and Bifidobacterium bifidum in patients suffering from major depressive disorder significantly alleviated depression26
- Thirty days of supplementation with a probiotic containing Lactobacillus helveticus R0052 and Bifidobacterium longum R0175 was able to not only reduce levels of cortisol – the main stress hormone – but also psychological distress in healthy human participants15
- Sixty days of Lactobacillus casei strain Shirota probiotic supplementation in chronic fatigue syndrome (CFS) patients led to a substantial improvement of anxiety symptoms28
- In comparison to the placebo group, medical students taking kefir with Lactobacillus casei Shirota for 8 weeks prior to an exam had lower rates of abdominal and cold symptoms, were less stressed as indicated by lower cortisol (stress hormone) levels, and had higher serotonin levels after the exam29
- Healthy women taking a milk product containing 5 probiotic strains for 4 weeks had detectable changes in activity of brain regions that control emotion and sensation30
- Three weeks of Lactobacillus casei Shirota probiotic supplementation in older adults (mean age 62) improved the moods of those individuals who initially reported a poor mood31
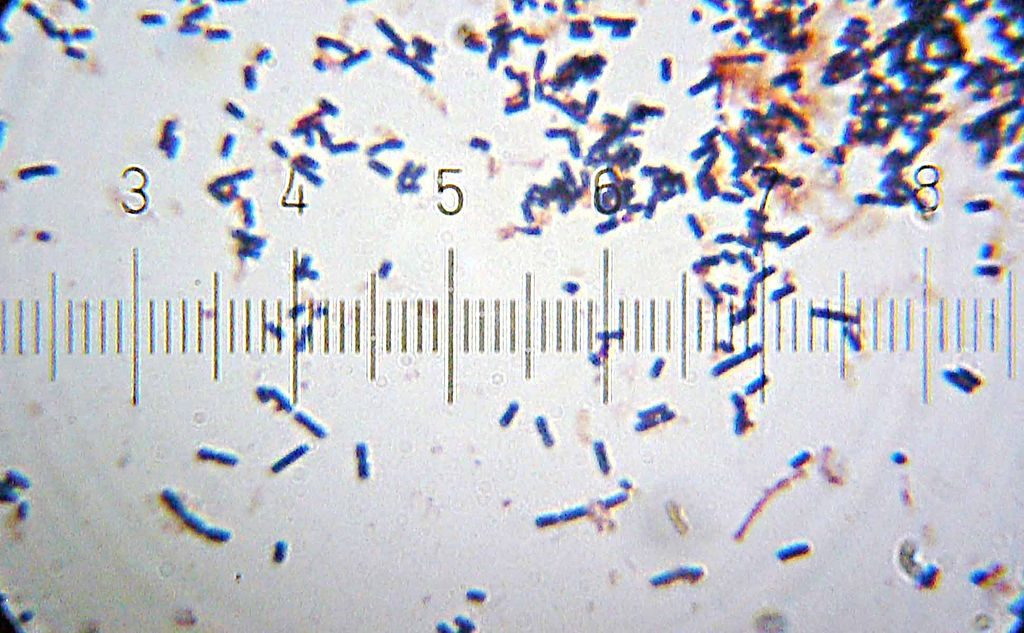
Bacteria classification
![By Doc. RNDr. Josef Reischig, CSc. (Author's archive) [CC BY-SA 3.0], via Wikimedia Commons](https://supplementsinreview.com/wp-content/uploads/2016/07/Lactobacillus_acidophilus_259_09_Lactobacillus_acidophilus_Döderlein_bacillus.jpg)
Bacteria are typically categorized by genus, species, and strain. The genus refers to a broader group of bacteria that share similarities, which is further broken down by species, and finally by strains – genetic variants of the same species. For example, the popular probiotic bacterium Lactobacillus acidophilus DDS-1 belongs to the Lactobacillus genus, species acidophilus, and strain DDS-1.32
The process of identifying which particular bacteria have psychobiotic potential has only begun. Thus far, the vast majority of such bacteria belong to the genus Lactobacillus and Bifidobacterium – the two names that already grace the covers of probiotic supplements.
Related Therapies
Prebiotics
For example, a study in healthy volunteers found that 3 weeks of supplementation with the prebiotic B-GOS decreased cortisol levels after waking up and boosted the processing of positive rather than negative information during a test. These findings suggest that some prebiotics are capable of not only reducing the body’s stress response, but also improving emotional processing.34
Meanwhile, a study in IBS patients demonstrated that taking 7 g of a trans-galactooligosaccharide prebiotic for 12 weeks, which raises levels of healthy Bifidobacterium, improved not just digestive symptoms, but also anxiety.35
Fecal Microbiota Transplants

While psychobiotics could be a potentially revolutionary therapeutic option for mental health, there is one more treatment method that holds just as much promise – fecal microbiota transplants (FTM).
FTM involves transplanting stool from one individual into another in order to restore the gut microbiota to a healthy state, and is already performed in people suffering from an overgrowth of the Clostridium difficile bacterium, curing the condition in nearly 90% of cases.36
If depression and other stress-related disorders are indeed linked to adverse changes in microbiota, then using FTM to restore it to a healthy state may be an even more potent treatment than psychobiotics.37
Conclusion
Although researchers stress the need for more extensive, well-designed human studies in both healthy and ill individuals, it’s clear that certain bacteria possess psychobiotic properties.38
Taking such psychobiotics is an effective way to boost the levels of beneficial bacteria in the gut, potentially improving stress, depression, anxiety, mood, and perhaps even overall cognitive function.
And while specifically-designed psychobiotic supplements do not yet exist, it is already possible to purchase probiotics that contain bacterial strains with psychobiotic potential, such as Bifidobacterium bifidum.
Once the pharmaceutical industry gets their money into psychobiotics research, a future of popping pills filled with bacteria to get over a depressing day or study for an exam may not sound so far-fetched.
Please can you tell me which probiotic to use I am 66 years old and am suffering from major depression and anxiety which I am convinced is because of my very poor gut health. I had cancer 8 years ago of the lining of my womb and had a radical hystrocemety followed by brachytherapy and since that have had huge amounts of uti’s and huge amounts of antibiotics and now my gut is in a mess I can see everything I eat in my stools and have to go to the toilet 5 and 6 times a day. I also feel so physically unwell I feel like my immune system is at a all time low and I am losing a lot of weight.
Please help thank you
@ Margaret
Try Lactobacillus plantarum. You can find it on Amazon. Best wishes.